Rights an individual has under HIPAA law
Unconscious bias is a pervasive yet often overlooked factor in the workplace. It can create a hostile environment and reduce productivity, while also impeding progress and creating divisions among coworkers. Explore the different types of unconscious bias, how they manifest in the workplace, and the actions that can be taken to combat them.
Patients have the right to request PHI restrictions
Under the Right to Request for Restrictions, individuals may request that their PHI not be disclosed to certain family members. A covered entity is under no obligation to agree to a request for restrictions. A covered entity that does agree must comply with agreed restrictions except for purposes of treating the individual in a medical emergency.

Patient Right to Access & Confidential Communications
According to the Right to Access, individuals have the right to access certain PHI in their preferred format–whether it be a digital or physical copy. Covered entities and business associates have 30 days to respond to the request with an approval or denial of access to the individual's PHI. HIPAA's Right to Confidential Communications requires covered entities to permit individuals to choose the way they receive communication of their PHI.

The HIPAA Privacy Rule gives individuals important controls over whether and how their PHI is used and disclosed. With limited exceptions, the Rule requires an individual’s written authorization before their protected health information can be used.
Under HIPAA. an individual has a right to file a complaint. A covered entity must have procedures for individuals to complain about its compliance with its privacy policies and procedures and the Privacy Rule. The covered entity must explain complaint procedures in its Notice of Privacy Practices. Individuals must be informed through privacy practice notices. Complaints can be submitted to the Company’s Complaint Official, or Health and Human Services (HHS). The organization may not retaliate against an individual for filing a complaint.
A right under HIPAA's Privacy Rule, known as the Right to Receive Notice of Privacy Practices, or NPP, gives individuals a right to be informed of the privacy practices of their health plans and of most of their health care providers. It also provides the right for individuals to be informed of their privacy rights with respect to their personal health information. This information is provided in the NPP. You must fulfill an individual’s request to receive your organization's NPP.
An individual has the right to find out about disclosures an organization has made to others about their PHI. This is called The Right to Accounting for Disclosures. The organization does not need to provide an accounting of all disclosures, as certain ones are exempt. For instance, disclosures to health care providers for treatment. The maximum disclosure accounting period is the six years immediately preceding the accounting request. Now, let's take a look at the standard accounting for disclosures when individuals do make a request.

The Right to Amend Patient PHI
The HIPAA Privacy Rule gives individuals the right to have covered entities amend their PHI. This is known as the Right to Amend. As a covered entity, in some circumstances you can deny the request for amendment. However, if the request to amend is denied, you must provide the individual with a written denial and allow the individual to submit a statement of disagreement, for inclusion in their record.
Patient Rights for PHI Privacy
It is important to know that your clients have rights regarding their PHI privacy. HIPAA sets forth a list of seven individual rights. They are:
Here are some myths to look out for:
- -
1. The Right to Access
- -
2. The Right to Confidential Communication
- -
3. The Request for Restrictions
- -
4. The Right to Amend
- -
5. The Right to Accounting for Disclosures
- -
6. The Right to Receive Notice of Privacy Practices also known as (NPP)
- -
7. The Right to File a Complaint

Using PHI for Fundraising or Marketing
With few exceptions, the the HIPAA Privacy Rule requires an individual’s written authorization before their PHI can be used for marketing. If a covered entity is paid directly or indirectly by third parties for marketing communications, then the authorization must state that the covered entity has been paid for the communication. The Rule distinguishes marketing communications from those communications about goods and services that are essential for quality health care. Certain parts of PHI may be used or disclosed for fundraising purposes. With each fundraising communication, individuals must be given a clear option to opt out of any further such communications.

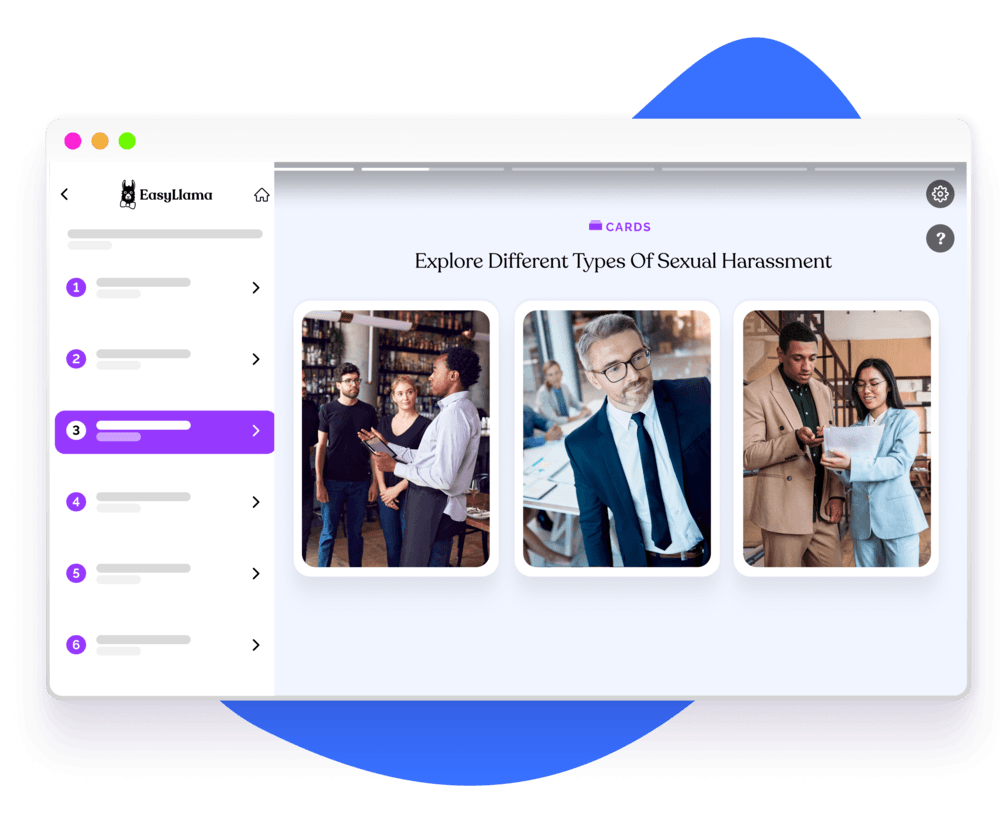
Helping over 8,000+ organizations create a safer, more inclusive company culture
EasyLlama’s online training course helps prepare employees to navigate HIPAA. This course provides an in-depth examination of how to respond to a breach of confidential data and the best way to protect your patients. The course covers: